- Several factors in people with HIV can contribute to an increased risk for high blood pressure
- Researchers studied 779 men, with and without HIV, to understand risks for high blood pressure
- High blood pressure and sleep disordered breathing were common among men with HIV
Disturbances in sleep can affect overall health and quality of life. Researchers have found that among people without HIV, sleep disordered breathing—also known as sleep apnea—is relatively common, affecting between 9% and 38% of adults in different studies. During sleep apnea, shallow breaths are taken or sometimes breathing pauses. This can happen because the airways become blocked. Sleep apnea is more common in men than women and in people who are overweight or obese or who have a family history of sleep disordered breathing, and in older people.
As sleep apnea causes shallow or interrupted breathing, the body gets less oxygen. This can cause people to feel tired the next day, have daytime sleepiness and develop a range of health problems over the long term, such as high blood pressure. Sleep apnea can be diagnosed after an overnight stay in a sleep clinic. During such a visit, sensors are attached to the body. These sensors can monitor breathing, heart rate, the amount of oxygen in the blood and other functions.
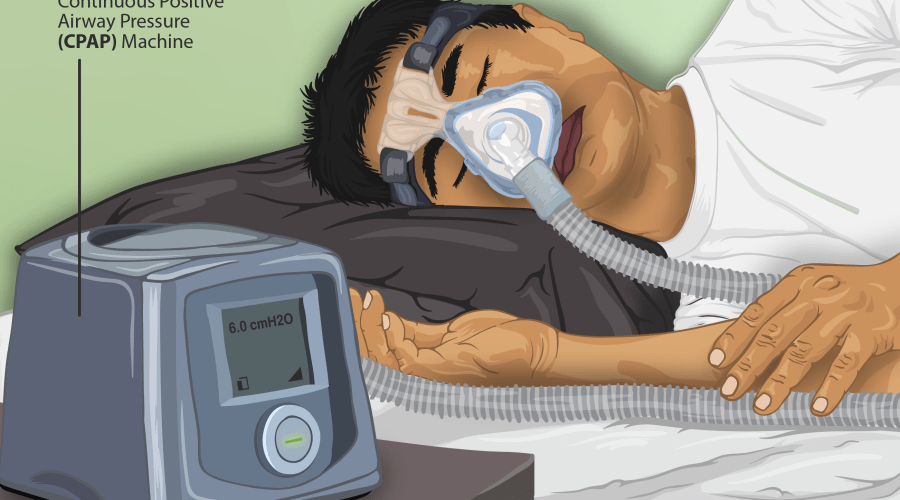
Doctors can prescribe interventions for sleep apnea, such as the use of small machines at night that provide continuous airflow via a small tube and mouthpiece or mask. This continuous airflow significantly reduces the risk of sleep disordered breathing. Studies have found modest decreases in blood pressure among people with sleep apnea who receive this intervention.
Why study sleep apnea and hypertension?
A team of researchers in the U.S. monitored men with and without HIV for sleep apnea and high blood pressure to find out if sleep apnea contributed to high blood pressure. The researchers were interested in these two conditions because risk factors for sleep apnea (being male, older, overweight or obese) are similar to risk factors for high blood pressure. According to the researchers, among people without HIV, “30% to 50% of patients with [high blood pressure] have sleep disordered breathing, and nearly 50% of patients with sleep disordered breathing have [high blood pressure].”
The researchers also stated that both “sleep apnea and [high blood pressure] are common in people living with HIV.” One U.S. study found that nearly 60% of men with HIV were diagnosed with sleep apnea. Another study found that about 25% of people with HIV had been diagnosed with hypertension. The reasons for the high rates of sleep apnea and high blood pressure in people with HIV are complex and may be related to underlying issues, such as excessive chronic inflammation.
A sleep study
The research team compared data from 436 men with HIV and 343 men without HIV. The men with HIV were younger, more likely to be smokers, and more likely to be people of colour compared to men without HIV. Most of the men with HIV (93%) were taking HIV treatment (antiretroviral therapy; ART) and had a suppressed viral load. On average, their CD4+ count was 700 cells/mm3. Commonly used classes of ART included integrase inhibitors, NNRTIs (non-nucleoside reverse transcriptase inhibitors) and protease inhibitors.
All of the participants received a package from the study centre. This package contained a recording device and sensors to measure airflow into the nose, the amount of oxygen in the blood, heart rate, brain waves, chest and abdominal movement during breathing, and so on. Participants were taught how to apply the sensors to themselves. The information gathered was relayed to the recording device, which in turn sent the data to the study researchers for analysis. Information for each person was captured over one night.
As part of a larger and ongoing study, participants visited the study clinic every six months to have their blood pressure and other measurements taken, to give blood and urine samples for analysis and to be interviewed about their health. The study was conducted between March 2018 and June 2019.
Results
High blood pressure was distributed as follows:
- men with HIV – 54%
- men without HIV – 56%
Rates of sleep apnea were high—82% in men regardless of their HIV status.
In further analysing the data, the researchers found that independently of each other, HIV and sleep apnea each contributed to an increased risk for high blood pressure. However, when these factors were analysed together in the same person, the combined effects of HIV and sleep apnea did not increase the risk for high blood pressure. That is, the risk of high blood pressure was similar among men with HIV and sleep apnea as it was among men with HIV alone or sleep apnea alone. This lack of an additive effect of sleep apnea and HIV on hypertension risk surprised researchers. One possible explanation that they proposed is that chronic HIV may somehow “saturate the mechanisms linking sleep disordered breathing to [high blood pressure].”
The researchers did not find any statistical links between different classes of ART and an increased risk for high blood pressure.
Screening and treatment
The researchers noted that sleep apnea was common among men with HIV and at risk for HIV. They encouraged clinicians to screen their patients (regardless of their HIV status) for sleep apnea and to treat it when found because “of the established benefits” that have been found in people without HIV in previous studies. The researchers stated that these benefits include improved blood pressure, reduced daytime sleepiness and improved quality of life.
Among people without HIV, sleep apnea is linked to an increased risk for cardiovascular problems such as heart attack and stroke. More research is needed to find out if sleep apnea can contribute to similar problems in people with HIV and the impact of interventions to improve breathing in people with sleep apnea in this population.
By Sean R. Hosein
REFERENCES:
- Punjabi NM, Brown TT, Abreu AR, et al. Sleep-disordered breathing and prevalent hypertension in men with and without HIV. JAIDS. 2023 Dec 1;94(4):349-354.
- Kunisaki KM. Do sleep disturbances contribute to comorbidities in HIV? Current Opinion in HIV/AIDS. 2023 Mar 1;18(2):81-86.
- McLaughlin MM, Durstenfeld MS, Gandhi M, et al. Cardiovascular health among persons with HIV without existing atherosclerotic cardiovascular disease. AIDS. 2023 Nov 15;37(14):2179-2183.
- O’Brien KE, Riddell NE, Gómez-Olivé FX, et al. Sleep disturbances in HIV infection and their biological basis. Sleep Medicine Reviews. 2022 Oct; 65:101571.
- Patil SP, Brown TT, Jacobson LP, et al. Sleep disordered breathing, fatigue, and sleepiness in HIV-infected and -uninfected men. PLoS One. 2014 Jul 3;9(7):e99258.
- Gutierrez J, Tedaldi EM, Armon C, et al. Sleep disturbances in HIV-infected patients associated with depression and high risk of obstructive sleep apnea. SAGE Open Medicine. 2019 Apr 8; 7:2050312119842268.
Source : CATIE
Get involved
Are you living with HIV/AIDS? Are you part of a community affected by HIV/AIDS and co-infections? Do you work or volunteer in the field? Are you motivated by our cause and interested to support our work?
Subscribe
Stay in the loop and get all the important EATG updates in your inbox with the EATG newsletter. The HIV & co-infections bulletin is your source of handpicked news from the field arriving regularly to your inbox.
